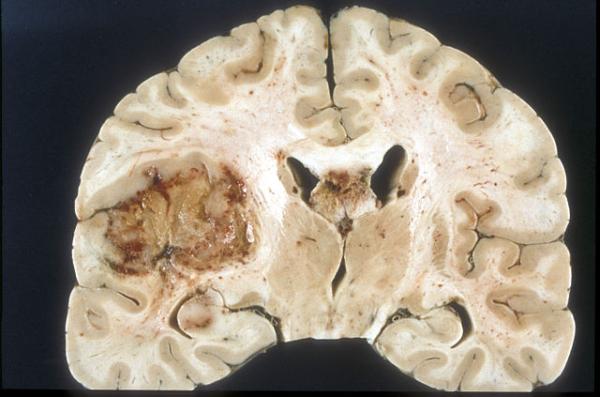
Glioblastoma multiforme (GBM), one of the most dreaded and deadly forms of brain cancer, has been on my mind recently because one of my dog-park friends was recently diagnosed with it. Characterized by aggressive growth and resistance to conventional treatments, GBM affects more than 14,000 Americans and claims approximately 10,000 lives each year. Even with intensive treatment — including surgery, radiation, and chemotherapy — the median survival time after diagnosis is 15 months, and only about five percent of patients survive beyond five years.
We desperately need new therapeutic strategies, and emerging research into advanced immunotherapy offers a glimmer of hope.
Among the most promising developments is a novel class of drugs called “DNA-encoded tri-specific T-cell engagers,” or “DTriTEs.” These cutting-edge molecules are designed to engage the immune system more effectively than traditional therapies, particularly against the heterogeneous and evasive GBM tumors. As explained below, the novel trivalent antibodies target two GBM antigens and a receptor on T lymphocytes.
Why Is GBM So Difficult to Treat?
GBM's resistance to treatment stems from its complexity and heterogeneity. The tumor is not just one type of cancer cell; it is a collection of diverse cells, each with different characteristics. This heterogeneity allows the tumor to evade therapies targeting a single marker. Efforts to harness the immune system to attack GBM have often been thwarted by the tumor’s ability to adapt and survive. For example, therapies targeting the epidermal growth factor receptor variant III (EGFRvIII) — a key protein often found in GBM cells — have shown only limited success due to the tumor’s variability.
Adding to the challenge, GBM’s location in the brain or spinal cord makes surgical removal difficult, and the blood-brain barrier limits the effectiveness of many drugs because it prevents them from getting to the site of the tumor. Despite decades of research, effective treatment of GBM is rare.
A New Approach: DTriTEs
To overcome GBM’s complex nature, a group of academic researchers based in Philadelphia have developed an approach called “DTriTEs,” a significant evolution in immunotherapy. Unlike traditional therapies targeting a single tumor-associated antigen, DTriTEs can simultaneously bind to multiple antigens while also activating T cells, the body’s immune warriors. Specifically, a recent published study describes using DTriTEs to target two GBM-related antigens — EGFRvIII and IL-13Rα2 — along with CD3, a receptor found on T cells, a subset of lymphocytes found in the blood.
This tri-specific design allows DTriTEs to address GBM’s heterogeneity: By engaging multiple antigens, they can target a broader range of tumor cells, reducing the likelihood that the cancer will escape treatment.
How Do DTriTEs Work?
DTriTEs function by creating a kind of bridge between T cells and tumor cells, turning the immune system into a multi-component weapon that attacks the cancer. When a DTriTE molecule binds to both a tumor cell and a T cell, it activates the T cell, prompting it to release antitumor molecules such as interferon-gamma (IFN-γ), tumor necrosis factor-alpha (TNF-α), and interleukin-2 (IL-2). These molecules not only kill tumor cells but also recruit additional immune cells to amplify the attack.
One of the most promising DTriTE constructs, known as DT2035, has demonstrated exceptional effectiveness in preclinical (animal) studies. In laboratory tests, DT2035 activated T cells and natural killer T (NKT) cells — specialized immune cells that play a crucial role in linking the innate and adaptive immune systems. Significantly, DT2035 achieved these results even in immune cells from GBM patients who had undergone extensive prior treatments, which often weakens the immune response.
Preclinical Success
In animal models, DT2035 showed remarkable results in controlling tumors. Mice treated with DT2035 experienced sustained tumor suppression, including in models designed to mimic the complex and diverse environment of human GBM. The therapy also demonstrated a longer-lasting effect compared to traditional protein-based regimens.
Notably, DT2035 activated both CD8+ “killer T cells” and CD4+ “helper T cells,” with the latter showing unexpected cytotoxic activity. This dual activation underscores the therapy’s ability to generate a robust and sustained antitumor response.
Further analysis revealed that DT2035 triggers polyfunctional T cells — cells capable of producing multiple types of antitumor molecules simultaneously. Such cells are considered critical for effective and lasting immune responses against cancer.
Why Multivalent Therapies Matter
The success of DT2035 highlights the importance of multivalent therapies — treatments that target multiple tumor markers simultaneously. GBM’s diverse tumor cells make it nearly impossible for single-antigen therapies to succeed, but by targeting both EGFRvIII and IL-13Rα2, DT2035 achieves broader coverage.
This multivalent approach also mitigates tumor escape mechanisms that enable cancer cells to evolve and to elude therapies that target a single marker. In preclinical models, DT2035 demonstrated superior performance compared to monovalent therapies, achieving long-term tumor control and improving survival outcomes.
Challenges and Next Steps
Although the results are promising, several challenges remain. Preclinical models, although useful, do not fully replicate the complexity of human GBM, particularly its immunosuppressive tumor microenvironment. Also, the long-term effects of sustained DTriTE expression — such as potential immune-related toxicity and other side effects — require further investigation.
Future studies will need to test DT2035 in diverse patient populations and explore its potential synergy with other therapies, such as immune checkpoint inhibitors. These inhibitors can remove the “brakes” on the immune system, potentially enhancing the efficacy of DTriTEs.
A New Frontier in GBM Treatment
Although the road to full regulatory approval is likely to be long, the progress made so far underscores the potential of innovative, multivalent therapies to tackle even the most formidable cancers. As research continues, DTriTEs may not only transform the treatment landscape for GBM but also pave the way for similar approaches in other cancers characterized by high antigenic diversity. They could represent a paradigm shift in cancer treatment.